
COVID era innovations will help shape the future for more equitable representation.
Oncology professionals from around the world attended the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting in June, one of the largest oncology research conferences of the year. Researchers presented breakthrough clinical trial data including new treatment options, symptom management and research in cancer care equity. The main theme of “Advancing Equitable Cancer Care Through Innovation” echoed the 2022 Cancer Day theme of “Closing the Gap” and offered a unique opportunity for the best minds in oncology to fully consider the problem in a face-to-face networking environment. It is a critical topic because currently, the inequities in who gets the maximum chance to survive a cancer diagnosis are frankly shocking.
Those left out include most low-and-middle-income countries (LMICs) as well as countless underserved communities and populations within high-income countries (HICs). It is estimated that by 2030, 75% of all premature deaths due to cancer will occur in LMICs, and the World Health Organization (WHO) has stated that global cancer rates could rise by 60% over the next 20 years unless cancer care in LMICs is ramped up. (Consider that even though an estimated 50% of cancer patients may require radiotherapy, there are still many countries without even a single radiotherapy machine.)
In HICs, those left behind include minorities, low-income communities, rural areas, the socially disadvantaged and the elderly. Where is the real benefit of innovative new therapies like precision medicine and immunotherapy when only a relatively few privileged populations have access? Some of the least served are children. WHO estimates that child cancer patients in LMICs have a less than 30% survival rate compared to 80% in HICs. That should simply not be acceptable. Inequities cover all aspects of care and research and have been made worse by recent pandemic conditions. (See Negative Effect of Pandemic on Cancer Survivorship)
The problem begins with research
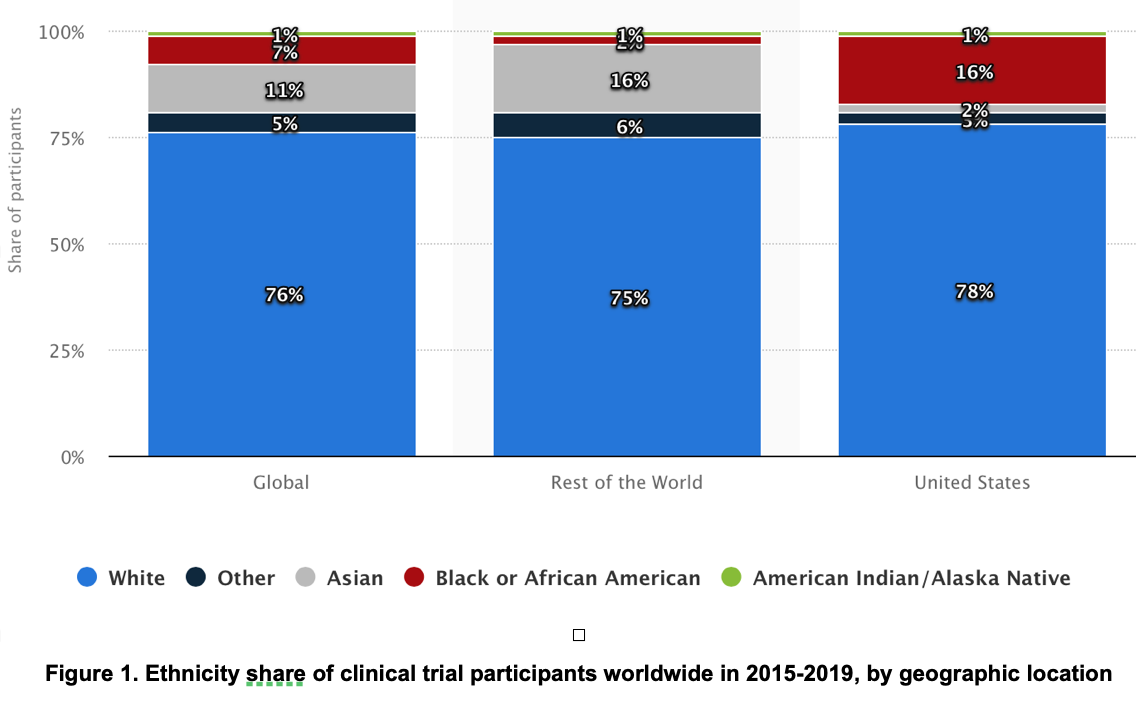
The problem begins at the research level. Clinical trials are conducted predominantly in HICs and on patient populations that far from represent the real ethnic diversity in the world. In May 2022, 87 US patient-representative organizations sent a letter to Congress urging legislation to improve diversity in clinical trials. They cited the fact that, “Despite racial and ethnic minority groups comprising nearly 40% of the US population, about 75% of participants in trials for drugs approved by the FDA in 2020 were white.” This is true across the globe. (Figure 1.) In addition, research eligibility criteria keeps existing cancer patients out of trials including older patients and many with health conditions such as diabetes and heart disease. Underrepresentation in research makes informed treatment decisions for all patients difficult, and, even when research is conducted more equitably, the cost of new therapies will most likely exclude access to the very patients who contributed to their development.
André Ilbawi, MD, of the WHO’s Cancer Programme, applauds the innovative approaches to cancer care representing paradigm shifts during the pandemic. “Historically, times of instability enable constructive change, and the pandemic has intensified the focus on health. A new chapter for cancer control is emerging,” said Dr. Ilbawi. “This is a unique opportunity to define what types of innovations will broadly improve health and well-being, enable more resilient health systems and reduce the profound inequalities that exist.” The pandemic saw rapid acceptance of decentralized care and trial operations including use of telemedicine, some home delivery of medications, ability of trial participants to get some treatments from community practices and remote consenting.
ASCO 2022 also highlighted a recent study showing the implementation of the Affordable Care Act’s Medicaid expansion was associated with nearly a threefold increase in the proportion of patients using Medicaid in cancer clinical trials by early 2020. “These findings are important because improved access to clinical trials for Medicaid patients provides greater access to the newest treatments. And it’s critical for improving confidence in trial findings applied to all patients, including those who are socioeconomically vulnerable,” said Joseph M. Unger, Ph.D., MS, of Fred Hutchinson Cancer Research Center in his ASCO presentation.
Etienne Brain, MD, Ph.D., senior medical oncologist at Institut Curie, in Saint-Cloud, France, honored with the 2022 B.J. Kennedy Geriatric Oncology Award at ASCO, said that within 20 years, 70% to 75% of cancer survivors will be aged 65 or older. He states that “Good data from clinical trials are sorely lacking for geriatric patients and, although there has been rapid progress with new targeted therapies in breast cancer, at most 15% of all patients enrolled in studies are older than 75.” He presented early results from ASTER 70s, one of the largest clinical trials conducted in the postoperative setting in women with breast cancer older than age 70.
ASCO also launched a data visualization tool showing the geographic distribution of systemic and socioeconomic factors influencing US cancer care delivery. This Interactive Map of Oncology, tracks US population-based oncology-related data by state and county from government and other authoritative sources overlaid with COVID-specific data. Physicians will be able to use demographics related to age, gender, cancer type and risk factors to better understand gaps that impact their patients’ health and well-being.
In his Opening Session Presentation, ASCO President Everett E. Vokes, MD, FASCO, said, “While the past half-century of research has transformed the care and treatment of our patients, deep-seated disparities remain between regions, economies and populations. We’ve seen exponential advances during COVID, from the record-breaking speed of developing vaccines and therapeutics to innovations in telemedicine and other novel ways to deliver care.” The future of cancer survivorship worldwide depends on research that is relevant to every country — every population — and therapies that are accessible to all people regardless of place or status. Innovations must be democratic to truly shift paradigms in the care and treatment of all cancer patients.



